Mother-Newborn Intensive Care Units and Small and Sick Newborn Care
Why is Care of Low Birthweight Infants Crucial?
Every year, approximately 20 million babies—15% of all births—are born with low birthweight (LBW). Over 70% of all newborn deaths occur in this vulnerable group. Interventions to reduce mortality in LBW infants are crucial if countries are to attain the Sustainable Development Goal of reducing neonatal mortality to less than 12 per 1,000 live births by 2030.
Kangaroo Mother Care

Photo Courtesy: Safdarjung Hospital, India
Among the various interventions to improve survival among LBW infants, kangaroo mother care (KMC) is among the most effective (40% mortality reduction). KMC involves keeping the baby in skin-to-skin contact on the mother’s chest continuously (until the baby no longer wants to stay in that position) and feeding the baby only breast milk. KMC not only helps babies survive, reducing problems such as hypothermia and hypoglycemia, but also promotes growth and long-term neurodevelopment. Currently, the World Health Organization (WHO) recommends initiating KMC in health facilities for all LBW babies who are clinically stable.
Unfortunately, the infants who are most likely to die in the first few days of life may not be eligible for KMC as per the current recommendation. Most newborn deaths occur in the first three days of life, when most babies weighing less than 2,000 grams are not considered stable. Thus, the 40% mortality reduction impact of KMC seen in the KMC studies would only be among survivors until this time. There is a critical knowledge gap regarding the effect on survival of initiating continuous KMC immediately after birth.
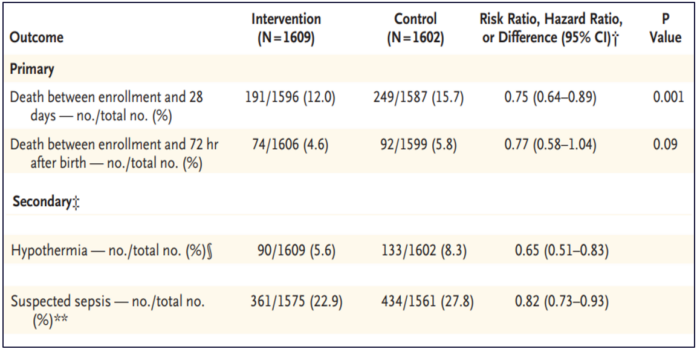
Immediate Kangaroo Mother Care
The WHO coordinated a large multicentric-multicountry clinical trial that recruited 3,211 LBW infants between 1.0 and 1.8 kilograms (kg) and their mothers in five hospitals with neonatal intensive care units (ICUs) in Ghana, India, Malawi, Nigeria, and Tanzania from December 2017 to January 2020. In the trial, LBW babies in the immediate KMC group were initiated with KMC with either the mother or a surrogate (until the mother was able to provide KMC) immediately after birth irrespective of stabilization. Mothers were able to provide about 17 hours of KMC per day to their small and sick newborns in the first few days of life in the ICU. Results of this study, published in the New England Journal of Medicine, showed that starting KMC early, rather than waiting for the LBW baby to stabilize, reduced mortality by 25%. The intervention provided to 27 babies saved one additional life. Thus, starting KMC immediately after birth has the potential to save up to 150,000 more lives each year, compared to the current recommendation of starting KMC only once the infant is stable. The table below shows the effects of immediate KMC on neonatal deaths (25% lower), hypothermia (35% lower), and clinically suspected sepsis (18% lower).
Mother-Newborn ICU
For the mother or surrogate to be available 24/7 for an LBW infant in the ICU requires converting the ICU to a mother-newborn ICU (M-NICU). This is a paradigm shift in neonatal care of the small and sick newborn. The M-NICU staff should be able to provide care for not only the LBW baby but also the mother. M-NICU facilities meet all of the mother’s basic needs, such as an area to warm food and eat, a toilet, and a shower.
Because the mother is continuously in close contact with her baby, she is able to help the nurses monitor the infant. The continuous presence of the mother in the neonatal ICU provides more opportunities for breastfeeding and reduces handling of the baby by health care providers.
One should not lose sight of the fact that the immediate KMC intervention cannot be provided in isolation. Infants who weigh less than 1.8 kg require a minimum package of high-quality care focusing on warmth, infection prevention, and provision of respiratory support.
What’s Next?
The WHO study was tweeted as a candidate for the most important neonatal trial in the 21st century. The study has the potential to bring about a paradigm shift in how small and sick newborns are cared for immediately after birth, laying the path for zero separation of LBW babies from their mothers.
The WHO will consider this intervention in the upcoming update of guidelines for care of LBW babies later this year. If recommended, neonatal health stakeholders around the world will have to consider how to rapidly scale up the intervention. Neonatal, obstetric, midwifery, and nursing professionals will need to embrace this paradigm shift in care of small and sick newborns. Governments globally will have to consider how to remodel current neonatal ICUs to M-NICUs and build M-NICUs when new facilities are constructed.
For centuries, the medical profession has separated mothers from their small and sick newborns. The results of the study highlight that restoring the mother to her rightful place at the center of her baby’s universe has profound benefits in improving the survival of small and sick newborns.
Dr. Rajiv Bahl, MBBS, MD Paediatrics, PhD, is newborn unit head and head of research in the Department of Maternal, Newborn, Child and Adolescent Health, and Ageing at the World Health Organization.
Dr. Suman Rao, MBBS, MD Paediatrics, DM Neonatology, is a professor of neonatology at St. John’s Medical College in Bangalore, India, and a consultant in the Department of Maternal, Newborn, Child and Adolescent Health, and Ageing at the World Health Organization.
